Philadelphia has firmly solidified its standing as the global capital of surgical innovation through unprecedented operations involving the separation of conjoined twins. However, the true breakthrough that forever altered medical history—demonstrating the staggering potential of human intellect paired with emerging technology—was the 1974 case of sisters Clara and Altha-Rodriguez Bidari. This landmark event at the Children’s Hospital of Philadelphia (CHOP) proved that the combination of masterful technique and a multidisciplinary approach could provide an independent life even in the most seemingly hopeless clinical scenarios.
In this article on iphiladelphia.net, you will discover the dramatic 1974 triumph of Philadelphia’s medical pioneers, where a team led by Dr. C. Everett Koop achieved the impossible—a groundbreaking 17-hour surgery to separate the Bidari conjoined twins, forever altering global surgical standards and granting two girls the gift of independent lives.
The Phenomenon of Conjoining: A Biological Puzzle and a Challenge to Science
When Clara and Altha-Rodriguez Bidari were born in the Dominican Republic in 1974, the world held its breath. They were more than just sisters; they were the physical manifestation of one of nature’s rarest and most complex biological mysteries. Conjoined twins are an anomaly that occurs when a fertilized egg begins to divide to create monozygotic (identical) twins, but for reasons still not fully understood, this process halts between the 13th and 15th days. The result is two distinct souls bound together by a shared body and intertwined vital systems.
For medicine in the mid-1970s, the Bidari sisters represented an ultimate test of both professional skill and human compassion. Philadelphia became the stage for an extraordinary drama where the stakes could not have been higher. Before this, successful separations involving complex organ sharing were exceedingly rare, often resulting in the disability or death of at least one of the infants.
The Anatomical Labyrinth: Understanding Ischiopagus Twins
The girls belonged to an exceptionally challenging category of conjoining known as ischiopagus. This meant their bodies were joined at the pelvis, positioned toward each other at an angle, creating a shared lower torso. The primary difficulty lay not in the external fusion of skin or muscle, but in the internal “knot” of vital organs that sustained both children.
Exhaustive examinations in Philadelphia revealed a daunting anatomical reality.
- Shared Digestive Tract. The girls’ intestines merged into a single canal, necessitating delicate surgical partitioning and reconstruction for each child.
- A Unified Liver. This massive, vital organ belonged to both sisters. Attempting to divide it in an era before modern laser scalpels or advanced synthetic sealants risked catastrophic, uncontrollable hemorrhaging.
- Intertwined Urinary and Reproductive Systems. Their internal anatomy was so deeply fused that diagnostic imaging of the time struggled to define where one organism ended and the other began.
By 1974, medical statistics for ischiopagus twins were bleak. Most attempts at surgical separation ended in the loss of both infants or required the ethically devastating “sacrifice” of one child to save the other. The Philadelphia medical team, fully aware of the grim history, chose a different path: a strategy dedicated to saving both lives.
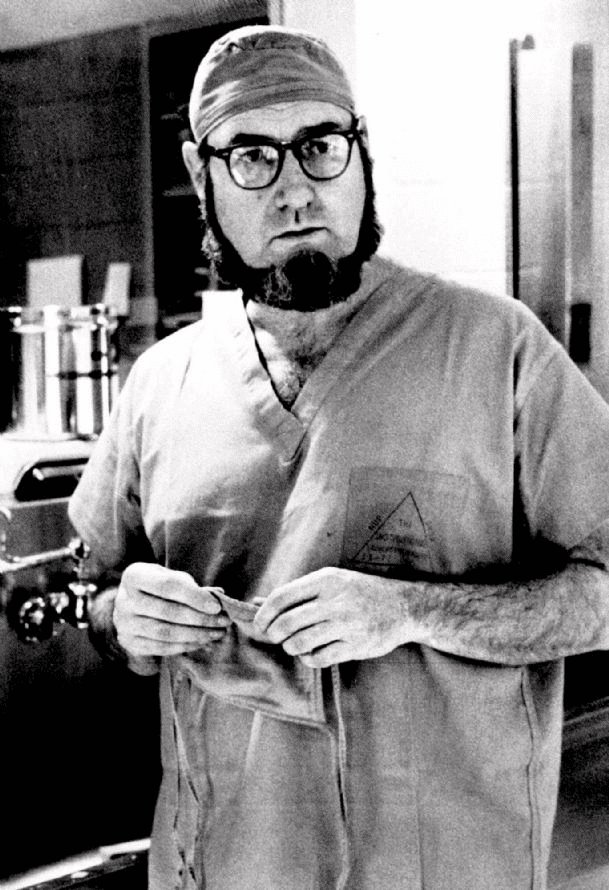
C. Everett Koop: The “Admiral of Surgery” in Philadelphia
At the helm of this monumental mission was Dr. C. Everett Koop, the Surgeon-in-Chief at the Children’s Hospital of Philadelphia. Koop was a man of legendary discipline and visionary thinking, whose authority in pediatric surgery was unparalleled (he would later serve as the U.S. Surgeon General). Koop understood that overcoming such a profound natural anomaly required more than the talent of a single surgeon; it required the coordinated power of a medical army.
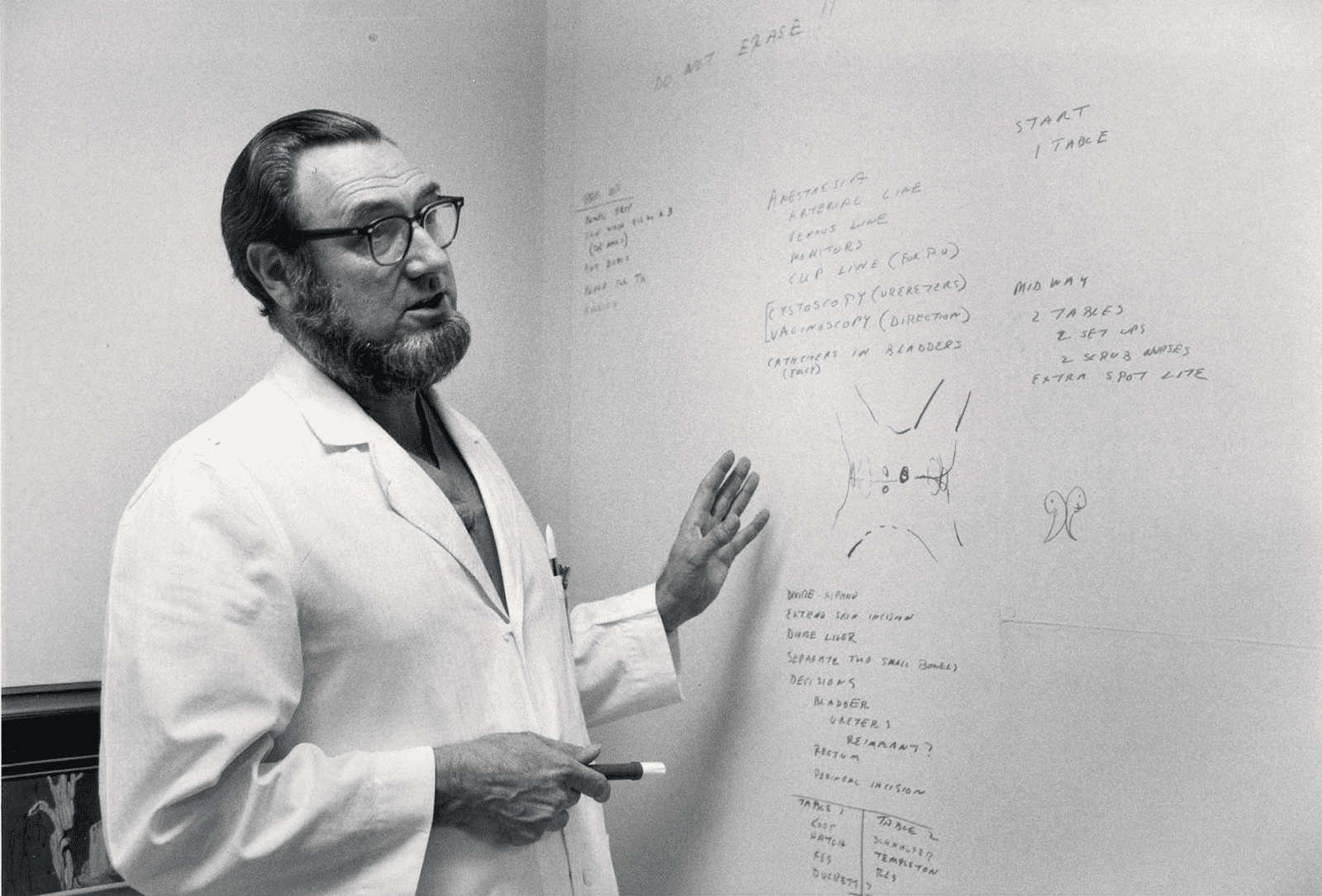
An unprecedented team of over 20 top-tier medical professionals—including urologists, orthopedists, plastic surgeons, anesthesiologists, and cardiologists—was assembled by Koop. For months leading up to the procedure, the team conducted intensive “dry runs.” They utilized mock-ups, models, and detailed X-rays to choreograph every minute of the upcoming operation. The great uncertainty was that no imaging technology in 1974 could provide a perfectly accurate picture of their internal structures. The doctors knew that the true anatomy of the twins would only be revealed once the first incision was made.
Seventeen Hours Between Life and Death: The Marathon Operation
The operation to separate Clara and Altha, which took place in September 1974, was a global sensation. Reporters from major international news outlets gathered outside the hospital, waiting for updates from the theater. It was a surgical marathon that lasted 17 consecutive hours.
The most critical and high-tension moment was the division of the liver. Without modern technological aids, the surgeons had to proceed with extreme caution; every millimeter of movement carried the risk of fatal blood loss. Once this stage was successfully completed, a second, equally daunting challenge began: the total reconstruction of two separate human bodies.
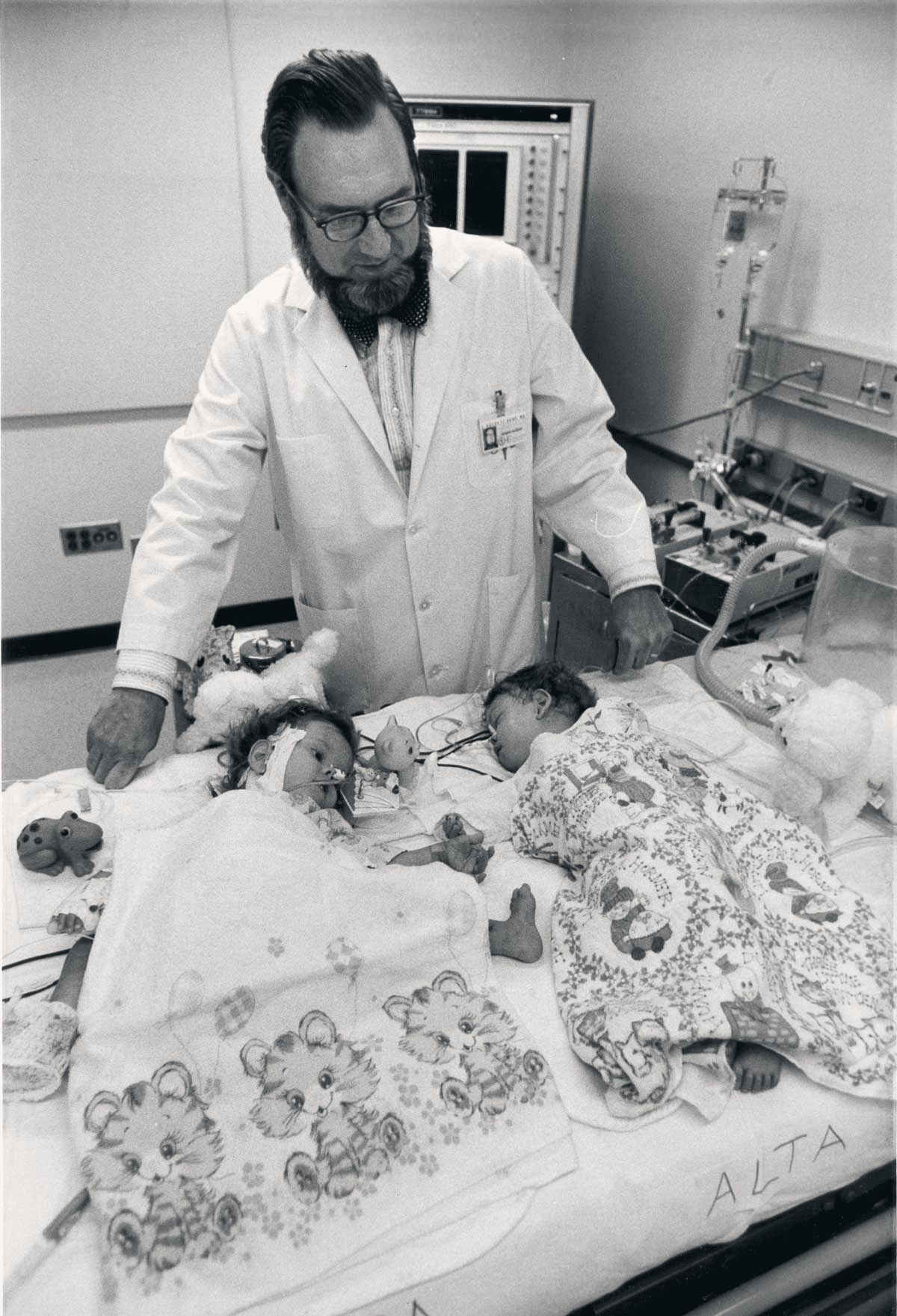
The surgeons did not just divide tissues; they essentially built functional pelvic systems for each girl from scratch, reconstructed their intestines, and ensured the integrity of their urinary tracts. The medical staff worked in two shifts, passing the patients from one specialized group to another under Dr. Koop’s vigilant oversight. When two separate gurneys were finally wheeled into the intensive care unit, cheers erupted in the hospital corridors. It was the moment science triumphed over a tragic biological error.
The Philadelphia Legacy: Setting a Global Standard
The success of the Bidari sisters’ operation was an absolute triumph for the Philadelphia medical establishment. The girls did not just survive; they thrived. After a long period of rehabilitation, they returned to the Dominican Republic and grew up to lead healthy, independent lives. The case of Clara and Altha-Rodriguez established several fundamental principles that remain the “gold standard” in modern global practice.
- The Multidisciplinary Model. The operation proved that treating the most complex pathologies requires the seamless integration of experts from diverse medical fields.
- The Ethics of Equal Value. The principle that each twin’s life is of absolute and equal value became the ethical benchmark for pediatric surgery worldwide.
- Reconstructive Innovation. The techniques for tissue and organ reconstruction developed by Koop and his colleagues during this surgery laid the groundwork for modern treatments for children born with severe congenital defects.
Philadelphia once again proved itself to be the city where the impossible becomes reality. The 1974 operation was not merely an entry in a medical journal but a profound humanistic act. It gave two individuals the right to their own separate futures and gave doctors around the world the confidence that intellect, preparation, and skill can overcome nature’s harshest.
Sources:
- https://cdispatch.com/news/c-everett-koop-former-surgeon-general-dies/
- https://www.lehighvalleylive.com/breaking-news/2013/02/koop_who_transformed_surgeon_g.html
- https://healthland.time.com/2013/02/27/remembering-dr-c-everett-koop-americas-doctor/
- https://www.nlm.nih.gov/hmd/conjoined/separation.html
